Pregnendione didn’t just show up out of the blue. Researchers started digging into steroid chemistry in the early twentieth century, and chemical curiosity led to exploring all sorts of derivatives from cholesterol and other basic structures in animal tissues. Teams in Europe and the US played with oxidation and reduction reactions, hunting for new hormones and possible pathways toward synthetic corticosteroids. Over the years, pregnendione became one of those basic building blocks in steroid research that helped crack the code for how the body’s hormones tick. Research from the 1940s laid out the bones of its structure, and people figured out methods to tweak it or convert it into compounds with real pharmacological muscle, such as cortisone and other glucocorticoids. Today, labs still circle back to pregnendione as they search for easier steroid synthesis paths, and its story keeps unfolding.
Scan through any chemical supplier’s catalog, and you’ll usually find pregnendione listed among basic steroid intermediates. Most researchers in pharmaceuticals or hormone analysis know to look for it during assay development or as a reference standard. The compound itself isn’t sold as a direct patient medicine but finds its value by serving as a tool in hormone pathway studies or as a key stop in synthetic chains aiming for important drugs. Its structure means it can function as a diagnostic reagent and as a step toward making more complex steroids.
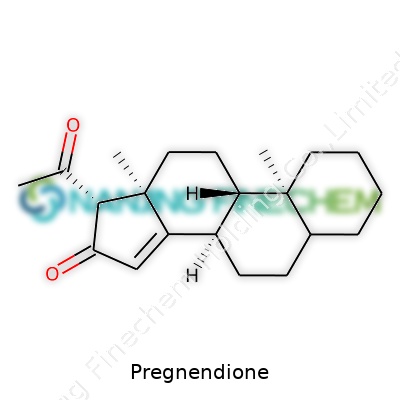
Pregnendione has a look that reminds a person of many basic steroids: it shows up as a solid, light powder with a faint yellow tinge. Chemically, it lands as C21H30O2 with a molecular weight just over 314 g/mol. Water doesn’t invite pregnendione in, but organic solvents like acetone or ethanol mix well. At standard temperature, it sits steady, without decomposing, and carries a melting point in the 125-130°C zone. Two keto groups pop up in its ring structure, giving it chemical angles for both reduction and further functionalization. It doesn’t let off much odor and keeps a stable profile if kept away from ferric ions, strong acids, or bases.
Reputable chemical suppliers label pregnendione in familiar glass vials, holding a few grams for research or production. Labels don’t hide details, giving CAS numbers (566-76-3) and specifying purity grades, generally above 97%. Documentation often extends to batch numbers, storage conditions (cool, dry storage), and safety advice. Shipping advice flags it as a non-hazardous substance for most purposes, but careful buyers still double check the MSDS before use. Every shipment includes a certificate of analysis, spelling out water content, specific optical rotation, and identification methods by NMR, IR, or mass spec.
Traditional ways to make pregnendione usually start with plant sterols or animal-derived cholesterol. Chemical oxidation of progesterone sets one path: treat it with mild oxidizing agents such as selenium dioxide or chromium trioxide, and the two spot ketone configuration marks out pregnendione clearly. Alternatively, microbiological routes employ specific bacterial strains, for example Rhizopus nigricans, which biotransform precursor steroids into pregnendione with fewer byproducts. Synthetic chemists prefer batch processes for scale-up, controlling temperature and pH to avoid side reactions, since yields drop sharply if reaction conditions stray. Improvements in green chemistry are squeezing out some of the older, harsher reagents, making the finished product cleaner and reducing downstream headaches.
Pregnendione often serves as a launching pad for making other steroid hormones, and its two keto groups act as magnets for chemists. Reductive amination, catalytic hydrogenation, or even Grignard reactions at the C-17 spot open up new doors for making analogs. Labs introduce halogen atoms or functionalize side chains, steering toward synthetic corticosteroids or progestins. Chemical tweaks extend to enolization under base, reduction at C-3 or C-20, or protection-deprotection cycles during multi-step synthesis. Pregnendione stands out for its flexibility, letting a single core compound branch off into dozens of clinically meaningful substances.
Pharmacopoeias and scientific articles tend to use synonyms almost interchangeably. "17,20-Pregnadione", "17,20-Dioxopregn-4-en-3-one", and "Pregn-4-ene-3,20-dione" show up in older and newer literature alike. Some reagent catalogs offer it as "Delta-4-pregnene-3,20-dione" or "Progesterone dione". IUPAC does its job by calling it 3,20-dioxopregn-4-ene, but the shorthand “pregnendione” remains the go-to for most chemists. These names keep researchers talking about the same molecule, even if spellings vary slightly by source.
Lab veterans know not to take even mild steroids lightly—personal protective equipment comes out, especially gloves and safety glasses. Unless handled on a big commercial scale, pregnendione doesn’t pose serious hazards, but a few milligrams on skin or inhalation deserves attention. Waste disposal sticks to standard protocols for organic compounds. Storage in cool, sealed places helps avoid degradation. If spills happen, wiping and disposal in the regular chemical waste stream works. No explosive or flammable features show up in its standard use, and long-term experience in academic and industrial labs confirms pregnendione’s fairly benign profile, as long as basic lab discipline sticks.
Pregnendione’s main role shows up in pharmaceutical and biomedical research. It forms a foundation for steroid hormone synthesis, letting medicinal chemists build everything from contraceptives to anti-inflammatory drugs. Clinical researchers keep it on hand for probing metabolic pathways, deploying it as a standard in enzyme studies, or using it in reference libraries for assay calibration. These applications ground pregnendione strongly in both lab and industrial setups, even though doctors won’t prescribe it by itself. I’ve seen labs in universities and industry reach for it during pilot projects aiming to construct new steroidal frameworks or probe early-stage hormone action.
Active research on pregnendione keeps pushing into better routes for synthesis, purer product, and easier modifications. Finding enzyme catalysts to mimic traditional chemical steps now grabs a big slice of grant funding. R&D teams look for streamlined processes with less waste creation and greener reagents, by trialing both chemical and microbial methods. In pharmacological circles, efforts keep circling back to its metabolite status and whether blocking its downstream products could lead to new therapies. The pace of papers and patents tells the story: pregnendione holds a place in the short list of must-have steroid intermediates for those searching for the next leap in hormone-based medicine.
Decades of animal and cell culture work lay out pregnendione’s basic safety profile. Acute toxicity lands fairly low, causing minor irritation at most. Studies run in rodents at higher dosages show no drastic changes in organ weights or bloodwork, though nobody recommends careless exposure or dumping. In vitro experiments indicate minimal cytotoxicity, but reproductive and developmental studies haven’t shown strong effects if dosed reasonably. Regulatory bodies classify it as low-to-moderate risk based on how much is handled and the intended use. This doesn't amount to a free pass, though; appropriate caution keeps everyone honest in handling and clean-up, and every new analog or derivative demands its own safety checks.
Pregnendione isn’t going away. As research on steroid biosynthesis ramps up, labs look harder for cost-effective, scalable reagents. Its role as an intermediate continues opening doors to analogs that could treat rare diseases, or fill supply gaps in the steroid market. Sustainable synthesis and biotechnological upgrades will probably reshape how it’s made and used. Industry might see it as a pivot for turning plants and microorganisms into micro-factories rather than sticking with older petrochemical starting points. Every new application, from improved diagnostics to designer drugs, still circles back to having a basic intermediate like pregnendione ready to go.
Pregnendione rarely gets much press. Folks outside of medical labs might not hear about it at all. Out of all the steroids produced by our bodies, this one sits quietly in the backstage, shaping the whole hormone scene. Pregnendione, for those curious, is a naturally occurring steroid in humans and other animals. It acts as a stepping-stone in the production of corticosteroids and sex hormones. Dipping into this compound gives a glimpse at how the body manages stress, fights inflammation, and keeps reproductive systems humming.
For people interested in what actually happens inside, Pregnendione matters because of what it turns into. The body converts it into either progesterone or 17α-hydroxyprogesterone. These two drive the production of cortisol, androgens, and estrogens. Cortisol gets released under stress and helps with metabolism, blood pressure, and immune protection. Estrogens and androgens define much of what we call puberty, fertility, and secondary sex characteristics.
Doctors will sometimes zero in on Pregnendione—especially if they suspect hormone imbalances or disorders tied to abnormal steroid production. For example, kids with congenital adrenal hyperplasia (CAH) may have mutations that disrupt the enzymes acting on Pregnendione. This leads to a pile-up of certain hormones and a shortage of others. Routine checks for Pregnendione levels can clue in specialists about what’s going wrong in adrenal glands or reproductive systems.
Pharmaceutical labs rely on Pregnendione, not so much for direct treatments, but as a building block for hormones that go into real therapies. Birth control pills, hormone replacement therapies, and even some treatments for cancer all draw from hormones spun out from this one molecule. Chemists in white coats work through Pregnendione as they synthesize specific steroids needed for these therapies.
Animal scientists also use Pregnendione in studies focused on pregnancy, fertility, and stress. Since it’s upstream of so many core hormones, tracking this compound helps map out how animal bodies adapt, mature, or react to illnesses.
Though it serves as a parent compound, Pregnendione isn’t something people get at the pharmacy. The body handles its own fine-tuning behind the scenes. Synthetic hormones made in labs mimic later-stage products like progesterone or cortisol, so patients never need to take Pregnendione itself. Tablets or injections offer more predictable effects, skipping the guesswork of how everyone’s body would process Pregnendione in the wild.
For anyone guessing why all this molecular talk matters, just look at the storm of side effects that pop up from hormone drugs. With more knowledge about steroid pathways, we get smarter at predicting reactions and tailoring doses. Maybe one day, drugmakers will develop finer tools to modulate what Pregnendione produces, dialing hormone signals up or down with less fuss. For families coping with hormone disorders, even tiny improvements here mean a smoother ride.
Sometimes it’s the low-profile chemicals that end up shaping the most critical processes in health and disease. Pregnendione’s story lives in the shadows, but the chain reactions it kicks off ripple through almost everything that makes us human.
Pregnendione doesn’t get called out much in ordinary conversations, but its importance in hormonal balance speaks loudly to anyone with experience in healthcare. I remember back in my pharmacist days, a handful of patients would ask about such compounds, wondering if a simple Google search could really cover all the bases. If only things were so straightforward. Hormonal support demands care, correct dosing, and a trustworthy routine.
Most folks hear “pregnendione” and figure it’s just another supplement, maybe something you buy with protein powders. This stuff works on a different level. Pregnendione connects to steroid synthesis in the body, playing its part in pathways that affect energy, mood, reproductive function, and metabolism. Anyone using it understands you can’t cut corners. Skipping advice from a doctor isn’t just unwise—it could spell trouble.
Let’s talk about how people actually take this compound. Typically, it comes as a capsule or tablet. The route seems simple, but the rules run deeper than just swallowing a pill with water. Pregnendione often requires a regular schedule to match the body’s own rhythms. Sticking to the same time each day makes everything smoother for hormones.
Eating habits play a part too. Some healthcare providers recommend taking it with food to dodge stomach discomfort. It’s tempting to think a missed dose isn’t a big deal, but inconsistent intake can mess up hormone levels in unexpected ways. This can bring unwanted side effects nobody wants to mess with—things like headaches or even mood swings.
I’ve seen patients chase after the “miracle blend” or seek something over-the-counter without checking with a real professional. Online forums and quick-fix guides don’t spell out the full story. Pregnendione isn’t Tylenol—it’s not for random, irregular, or self-adjusted use. The risks aren’t always obvious at first, but messing with hormones can spark a chain of unwanted events—think irregular cycles, sleep troubles, or even cardiovascular concerns.
People often think more is better, especially with supplements. Pregnendione doesn’t play by those rules. The amount and timing depend on a person’s medical profile, goals, and lab values. A doctor might order regular blood work to check how things are moving along, adjusting the dose as needed. I’ve had conversations where the plan changed because of shifting blood markers. Stick to the plan, and the chances of hitting roadblocks drop.
Many people stack supplements, especially those into sports performance. Pregnendione may react with other medications—including some used for mental health, blood pressure, or even antibiotics. Everything needs to be on the table during one of those “bring your pills” appointments at the doctor’s office.
Honest conversations with a healthcare provider always win out over guesswork. Keep a log of reactions, follow instructions, and never rush changes. With hormone-related products, there’s no trophy for going it alone. Controlled, steady use backed by regular check-ins turns uncertainty into confidence. That’s the difference between using Pregnendione wisely and rolling dice with your body.
Pregnendione, a steroid hormone, doesn’t usually show up in casual conversation. Yet, anyone going through issues with hormones or researching treatments for certain medical problems might stumble across its name. It sits in the corner of steroid chemistry, quietly influencing things behind the curtain. My own run-ins with hormone topics—mainly through people close to me who’ve needed hormone therapy—have taught me one thing: changes in natural body chemistry rarely travel alone. They drag along side effects.
People sometimes take pregnendione for medical reasons, sometimes related to hormone imbalances or research studies. Side effects tend to tag along with steroid-based substances, often related to the body’s own hormones getting thrown out of balance. Here’s what commonly shows up, based on studies and patient stories:
Certain side effects demand attention. High doses or long-term use can affect liver health, stirring up enzyme levels that doctors need to monitor. In rare cases, pregnendione use might worsen existing heart or kidney issues. People with a medical history in these areas shouldn’t brush off weird symptoms, even if they seem minor at first.
Doctors should walk anyone considering pregnendione through regular check-ins. Blood tests, honest conversations about mood or cycles, and patience for close observation work better than guesswork. If a side effect outweighs the original benefit, it’s time to talk about switching approaches. Adjusting the dose or stopping the treatment can help the body find balance again. Support from friends and family can bring comfort since talking about side effects sometimes feels embarrassing.
Digging up honest, reliable information on hormone treatments helps people make better decisions. If something feels off—changes in mood, strange aches, or a new rash—raising the alarm sooner helps prevent bigger trouble. From my own perspective and what I’ve watched others go through, listening to how the body reacts holds more wisdom than most instruction leaflets.
Pregnendione doesn’t get the same attention as the better-known hormones, but it’s a steroid closely related to progesterone. Some folks bring it up as a supplement or in the context of hormone therapy, sometimes thinking it helps balance hormones or supports pregnancy. But words like “natural hormone” mean little if we don’t know what they actually do inside us, especially during pregnancy or breastfeeding, when little things can make a big difference.
Whenever a new substance pops up and someone wonders if it’s okay during pregnancy, the honest answer often comes from what studies actually say. For pregnendione, not much real research has been done in people, and most medical guidelines skip over the topic entirely. In medicine, scientists dig deep into safety by running trials, gathering data across groups, and following up with people over years. With pregnendione, studies just aren’t there. If something hasn’t been looked at closely, calling it safe feels like guessing in the dark.
There’s a sort of built-in caution during pregnancy since so many changes are happening. The placenta can move things from a mother’s blood to the baby’s, and even small doses of some substances have triggered problems. History is full of examples—thalidomide and even high levels of vitamin A come to mind. Experts tend to hold medications and supplements back from expecting and nursing parents unless the benefits stand out and risks are clearly understood.
Over-the-counter supplements don’t always go through the same tough checks as prescribed drugs. Makers sometimes list ingredients loosely, and batches may differ. Pregnendione could be mixed with other steroid-like compounds. If a bottle comes with vague promises and no solid safety data, trusting it with a pregnancy feels risky. It gets trickier with breastfeeding, since small amounts of hormones could slip into milk, and developing babies are extra sensitive.
Obstetricians and pediatricians tend to stick with medicines and supplements that come with decades of observations. Pregnendione hasn’t made their approved lists for pregnancy or breastfeeding. Trusted resources such as the American College of Obstetricians and Gynecologists or the LactMed database offer no recommendations supporting its use. FDA guidelines add anything that hasn’t been proven safe to the “avoid unless necessary” list.
There’s a lot of pressure to feel like every part of pregnancy or breastfeeding should be perfect. Promises of energy, hormone balance, or easier milk production sound tempting. Social media, blog posts, and some online forums share stories that selling points work, but stories don’t replace data. Years ago, I watched close friends chase after every “natural” remedy, only to learn later that most just emptied their wallets or, worse, caused unexpected symptoms. When there’s doubt, waiting for solid information matters more than a hunch or a sales pitch.
Folks wondering about pregnendione need straight answers, not marketing. During pregnancy or nursing, the safest bet comes from using only what a trusted doctor suggests. If you come across a new product, press the pharmacist or OB for details, and don’t settle for shrugs or guesses. Scientists owe parents clear, long-term studies about what helps and what could really hurt. Until then, sticking with tried-and-true options protects both parent and baby. With so much at stake, playing it safe beats trusting the unknown every time.
Pregnendione isn’t the kind of medication you’ll run into at a local pharmacy unless you know your way around steroid hormones. It sits among a family of compounds that play big roles in how our bodies handle inflammation, stress, and even energy. I remember seeing a friend’s prescription bag filled with things I couldn’t pronounce, meant to handle menopausal symptoms after every other option seemed to hit a wall. The more I dug into what some of these hormones do, the more it became clear: sharing space on a schedule with other pills invites some friction.
Anyone tracking the growing list of personal meds knows the drill—you have to ask if something new clashes with the regulars. Steroid hormones like pregnendione can shake hands with all sorts of drugs, often changing how the body puts those drugs to work. Take blood thinners, seizure medicines, or even something as basic as pain relievers. The story keeps repeating: throw a hormone or steroid into the mix, and levels of other meds might shift, sometimes dangerously.
A classic example jumps out with things like warfarin. Add a hormone-related drug, and suddenly clotting risk gets unpredictable. There’s real science behind it. Pregnendione tweaks liver enzymes, the same ones that clean other medications out of the system. So blood levels of those drugs can shoot up or dip without warning. Experiences from folks juggling several prescriptions show how easy it is to slip into trouble simply because a new steroid start-up seemed harmless enough.
Over the years, I’ve watched people double-checking their pill planners, not just for missed doses but because their doctors warned about drugs “competing.” The problem isn’t just theory—it’s people waking up with huge bruises because their blood’s too thin or realizing their insulin isn’t working as usual. Doctors often go over the list of potential side effects, but there’s something about steroids that sneaks up on people. The body masks discomfort until something serious surfaces.
Digging a bit, research shows that patients with autoimmune disease, diabetes, or even epilepsy face the highest stakes. Those steroid-like compounds can mess with how anti-seizure meds work or change blood sugar control. It’s not really about scare tactics; it’s the kind of thing you only learn after the fact if nobody thinks ahead.
People already taking medications deserve better than guesswork. My advice always starts with honesty: tell your doctor exactly what you take—including vitamins or herbal stuff that never seems important until it is. Pharmacists have told me the same—they’d rather check a possible clash than clean up a mess after it happens. Tools like medication review apps and pharmacy consultations help a lot.
The bigger lesson is remembering what’s on your list isn’t always safe to add to. Regular blood tests and open talks with your healthcare team aren’t just about checking boxes. They’re about catching trouble before it starts. The world of hormone-based medications isn’t simple, but staying involved and asking tough questions can make all the difference.
Medication labels say a lot, but real safety lives in the details. Pregnendione may not headline the nightly news, but for the people taking it—or sharing a medicine drawer with it—interaction checks aren’t optional. They’re what keep a careful balance in an otherwise hectic routine.
| Names | |
| Preferred IUPAC name | 8,11,9(10)-Pregnatriene-3,20-dione |
| Other names |
delta(5)-Pregnene-3,20-dione Pregenolone 17β-iso-Androstene-3,20-dione 3,20-Pregnendione |
| Pronunciation | /prɛgˈnɛn.dɪ.oʊn/ |
| Identifiers | |
| CAS Number | 566-97-2 |
| Beilstein Reference | 3580965 |
| ChEBI | CHEBI:28689 |
| ChEMBL | CHEMBL1429 |
| ChemSpider | 68209 |
| DrugBank | DB01545 |
| ECHA InfoCard | ECHA InfoCard: 100.203.293 |
| EC Number | 1.1.1.145 |
| Gmelin Reference | 64314 |
| KEGG | C02336 |
| MeSH | D004556 |
| PubChem CID | 92274 |
| RTECS number | KM2975000 |
| UNII | 1U1QTN40SY |
| UN number | UN2811 |
| Properties | |
| Chemical formula | C21H30O2 |
| Molar mass | 312.409 g/mol |
| Appearance | White to off-white crystalline powder |
| Odor | Odorless |
| Density | 1.07 g/cm³ |
| Solubility in water | Slightly soluble in water |
| log P | 2.5 |
| Vapor pressure | 6.93E-07 mmHg at 25°C |
| Acidity (pKa) | 4.07 |
| Basicity (pKb) | 4.67 |
| Magnetic susceptibility (χ) | -654.7e-6 cm^3/mol |
| Refractive index (nD) | 1.583 |
| Viscosity | Viscous liquid |
| Dipole moment | 2.94 D |
| Thermochemistry | |
| Std molar entropy (S⦵298) | 333.5 J·mol⁻¹·K⁻¹ |
| Std enthalpy of formation (ΔfH⦵298) | -134.9 kJ/mol |
| Std enthalpy of combustion (ΔcH⦵298) | -1747.8 kJ/mol |
| Pharmacology | |
| ATC code | G03BA04 |
| Hazards | |
| Main hazards | Suspected of damaging fertility or the unborn child. |
| GHS labelling | GHS02, GHS07 |
| Pictograms | GHS07 |
| Signal word | Warning |
| Hazard statements | H302: Harmful if swallowed. H315: Causes skin irritation. H319: Causes serious eye irritation. H335: May cause respiratory irritation. |
| Precautionary statements | Wash thoroughly after handling. Wear protective gloves/protective clothing/eye protection/face protection. If skin irritation occurs: Get medical advice/attention. Take off contaminated clothing and wash it before reuse. |
| NFPA 704 (fire diamond) | 2-1-0 |
| Flash point | 166.7 °C |
| Autoignition temperature | Autoignition temperature: 500 °C |
| Lethal dose or concentration | LD50 (rat, oral): 2500 mg/kg |
| LD50 (median dose) | LD50 (median dose) of Pregnendione: "5000 mg/kg (rat, oral) |
| PEL (Permissible) | Not established |
| IDLH (Immediate danger) | Not established |
| Related compounds | |
| Related compounds |
5-Dihydroprogesterone Deoxycorticosterone Hydroxyprogesterone |