Pregnan-3,20-dione, known better in clinical and research circles by the name “progesterone,” has roots running deep into the early days of hormone discovery. This molecule shows up time and again as researchers looked for answers in reproductive health and methods to support pregnancies at risk. The 1930s brought a wave of work on this compound, driven by hard scientific curiosity mixed with the human desire to solve practical health problems. Chemists in European labs, chasing both fame and a genuine urge to understand the body’s processes, managed to pin down this steroid. They worked through messy, labor-intensive extraction from animal glands and later turned to synthetic methods that still inspire respect for their creativity. The journey from animal extract to bulk synthesis never ran smoothly, but it unlocked doors to treatments that changed reproductive medicine.
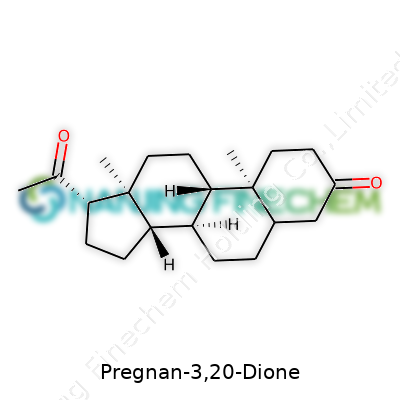
Taking a closer look at the molecule itself, pregnan-3,20-dione, the technical term rolls off the tongue a bit less easily than “progesterone,” but it carries its own weight. This molecule falls under the steroid family, sitting at the crossroads of biochemistry and pharmaceutical production. It takes the form of a white or almost white powder, showing up in labs and on pharmacy shelves in crystal form. Solubility often throws the first hurdle in laboratory setup; water does little for it, so folks working with it turn to alcohol, acetone, or oils. Its melting point hovers around 126°C, which plays into how manufacturers dry and store it, and its chemical stability means it can survive rough handling better than some other hormones. All this might sound dry, but for anyone aiming to turn raw powder into a medicine meant for people, these physical quirks make the difference between a safe pill and a useless one.
Technical documents for pregnan-3,20-dione pack pages with details—chemical formula C21H30O2, CAS number 57-83-0, and purity grades measured down to tenths of a percent. Pharmaceutical suppliers argue over whether their batch holds 99.5% or 99.8% purity, each percentage point a badge of production pride and a key fact for researchers. Labels also flag storage instructions: cool, dry, shielded from sunlight. Handling gets outlined in brutal detail, since a careless hand could let humidity sneak in where it doesn’t belong. On the shelf or inside a production plant, slips in labeling or mismeasurement can stop a shipment or compromise a batch. In this business, precision is currency and accountability isn’t negotiable.
Early factories looked to animal tissue for their source. Workers processed pounds of cow ovaries or pig glands, knowing that a fraction of a gram of hormone would mean hours of work. This model, unsustainable at scale, led the way for chemists to chase down plant sources. Mexican yams, especially those carrying diosgenin, offered a solution. Laboratories developed ways to convert plant sterols into pregnan-3,20-dione through a mix of oxidation, isomerization, and purification processes. The industrial push refined the method into a science of its own, with control over solvents, pressure, and catalysts gaining more value than brute labor. Technology’s march never waits, and now computer-monitored reactors fine-tune every batch, letting giants pump out thousands of doses with almost frightening consistency. None of this escapes regulation, since mishaps can breed contamination or ineffective product, and public trust gets lost faster than it’s built.
Pregnan-3,20-dione doesn’t just sit on the shelf; researchers keep asking more from it. Hydrogenation smooths out double bonds, veering toward new analogues with different biological profiles. Aldol condensations and ring modifications pop up in patents, each promising tweaks that sharpen or dampen certain effects. Some of these pathways end up in contraceptives, while others lead to treatments for menopause, or even oddball uses in animal health. It’s rarely a straight line—a small change in one step can flip the safety or function of the resulting compound, which holds back some otherwise promising ideas. Yet, real breakthroughs have come from this stubborn habit of chemical experimentation, with new generations of steroid medicines facing off against older, less predictable drugs.
The main name, Pregnan-3,20-dione, often gets shuffled aside in favor of “progesterone” in the clinic. Still, chemistry texts roll out synonyms such as corpormon, luteal hormone, and progestin, with each marking a different use case or company label. Specialty chemical catalogs list alternate identifiers—Pregn-4-ene-3,20-dione among the most common. Each synonym throws a lifeline to a chemist scanning the literature or a doctor considering treatment options, making it clear that behind every alias, the backbone remains the same. Familiarity with these names shortcuts confusion in research and practice, especially across languages and regulatory zones.
Every gram handled demands respect. Old horror stories about hormone exposure—lab workers dealing with symptoms they never signed up for—linger in the background. Gloves, fume hoods, and careful waste disposal all get drilled into staff from day one. Industrial rules spell out exposure limits, not just for the safety of workers but for anyone down the line. Progesterone may help millions, but mishandled, it brings real risks of skin or eye irritation, and chronic exposure can trigger subtle or lasting endocrine changes. Facilities and companies hold tight to safety data sheets and audit trails, understanding that any misstep can draw regulators’ attention or worse, harm people. There’s no shortcut to responsibility here, especially with set standards enforced from batch raw material delivery through final tableting and shipment.
Few molecules fill as many shoes as pregnan-3,20-dione. Most people recognize it for its front-line role in women’s reproductive health—hormonal therapies, oral contraceptives, treatments for infertility and preventing preterm labor. Yet it finds its way into veterinary treatments and research protocols. Through its key effects on preparing the uterine lining and regulating menstrual cycles, it supports millions who need medical interventions to live life on their own terms or bring pregnancies to term. Beyond direct use, the same backbone structure underpins whole families of drugs, including corticosteroids and androgens, reaching far outside the original field. In many ways, its importance in the pharmaceutical landscape keeps growing, as both stand-alone therapy and as a building block for new medications.
Science rarely stands still. Research teams chase every angle, searching for ways to improve delivery or reduce side effects. Formulations keep getting upgraded: slow-release injections, subdermal implants, and better oral options aim to make real-life use as hassle-free as possible. Clinical trials keep exploring its place in therapies beyond classic hormone replacement, from cancer prevention to neuroprotection. Academic curiosity meets industry efforts, backed by advances in chemical engineering and biotechnology. Some of the most exciting work circles around tweaking the molecule to create new analogues targeting orphan diseases. Even small steps here circle back, shaping dosing regimens and rewriting the rulebook for hormone therapies.
Every boost in usage shines a brighter light on toxicity questions. Researchers, regulators, and prescribers have learned not to take hormone safety for granted, drawing on decades of monitoring for unintended effects. Standard studies in rodents and primates plot long-term use against cancer risk, reproductive health, and subtle effects on immune systems. Real-world data—what happens once a drug reaches people across continents—feeds into registries tracking reactions, allergic triggers, and risk of blood clots or cancer. Surveillance stays tight because even the best intentions can turn bad if warning signs go unnoticed. Pharmacies and clinics flag possible side effects, training staff to spot red flags before they turn into real harm.
Future prospects for pregnan-3,20-dione don’t just rest on recycled uses. Demand grows for greener, more efficient synthesis, and there’s a push to slash manufacturing waste and move away from harsh solvents altogether. With shifts in public attitudes around hormone use, research leans into developing targeted therapies that promise benefits without the catch-all side effects of old formulations. Digital health, personalized medicine, and even gene editing technologies open fresh chapters in applying age-old hormones in modern settings. The molecule may stay the same in core structure, but its applications and manufacturing methods keep being reshaped by technology, regulation, and the shifting real-world landscape of health care. People will keep looking for better ways to solve today’s problems, drawing on what pregnan-3,20-dione can offer while keeping eyes wide open to both its promise and limitations.
Step inside a pharmacy or a medical research lab, and Pregnan-3,20-Dione doesn’t roll off the tongue the way aspirin or caffeine might. This tongue-twister is better known on the street as progesterone, a hormone that keeps the wheels of reproduction turning. Talking about hormones can sound like a game of chemistry Scrabble, but progesterone—this very compound—shows up constantly in conversations about fertility, periods, and even cancer research.
Many folks think of progesterone as the “pregnancy hormone,” but narrowing the story to pregnancy ignores how often this chemical acts behind the scenes. Every month, it helps prep the lining of the uterus so a fertilized egg might stick. Without the right levels, a woman’s cycle may feel off-balance, and pregnancy might not start or last. This isn’t some rare situation. A lot of women with fertility struggles end up talking about progesterone at their doctor visits.
Doctors don't just use Pregnan-3,20-Dione to support pregnancies. Think about birth control pills. Some types use synthetic copies of natural progesterone to keep the body from ovulating. The goal: no egg, no baby. Others rely on it to regulate periods for teens with irregular cycles or anyone with endometriosis, where tissue grows outside the uterus. Heavy periods, missed periods, even severe PMS often connect back to how progesterone works—or doesn’t work—in the body.
Scan through cancer research, and progesterone pops up again. For some patients with breast or uterine cancers, treatments include drugs that block how the hormone acts, cutting off a fuel supply for certain tumor cells. This isn’t perfect—side effects hit hard and not all tumors listen—but it’s one more angle in the multi-pronged attack on cancer.
It surprises a lot of folks that progesterone also connects to bone health. As estrogen gets most of the spotlight for osteoporosis, a quiet pile of studies shows progesterone helps keep bones strong, especially post-menopause. The science here isn’t settled, and diet, exercise, and genetics still take front seat. Still, it’s one of those corners of medicine that’s heating up as researchers look for safer, more natural ways to prevent bone loss.
Using Pregnan-3,20-Dione isn’t always straightforward. Synthetic versions—progestins—don’t act exactly like the natural stuff your body makes, and side effects aren’t rare. My neighbor once struggled with mood swings and fatigue after her doctor swapped out one hormone med for another. Doctors double-check tests before prescribing it, considering a patient’s history with clots, strokes, or certain cancers.
For everyone watching hormone levels at home, over-the-counter “progesterone creams” create confusion. Many don’t do much, as research shows they rarely reach the bloodstream in real amounts. This misleads people and wastes money that could pay for more dependable medical care.
Progress demands deeper research and better education. Clinicians could listen more closely to patient stories, tracking hormone side effects and tailor treatments instead of relying on one-size-fits-all hormone cocktails. Pharmacies and online retailers could label supplements more clearly and keep wild promises off the package. More funding means faster answers about how progesterone influences mood, sleep, and risk of disease.
In the end, Pregnan-3,20-Dione may not get glamorous press, but it shapes daily lives, medical care, and even new treatments. Putting more honest talk and smarter science behind how we use it could turn everyday hormonal chaos into something much easier to live with.
Pregnan-3,20-Dione goes by a simpler name in most conversations: progesterone. This hormone sits right in the middle of women’s health, keeping things like pregnancy and periods moving along the way nature meant. Doctors reach for it in a bunch of situations—helping with fertility, easing menopause symptoms, even balancing hormones during gender-affirming care. Like any hormone, it brings its own baggage. People want to know what kind of side effects to expect before saying yes to it.
Taking any hormone sets off a string of reactions through the body. With progesterone, some of the most common side effects show up quick. I remember a friend getting prescribed it for heavy cycles. She called me a week after starting, barely able to keep her eyes open during our phone call. Fatigue can slam hard, and it doesn't just mean feeling sleepy—it hits the body so folks reach for coffee mugs by midmorning. Headaches join the party for some, and bloating rolls in like an unwanted guest. All that fluid doesn’t move through easily, and clothes fit tighter for a while.
Mood swings deserve a mention, too. I’ve heard from more than one person that progesterone makes patience wear thin or brings out the tears over old sitcom reruns. These symptoms have scientific backing: this hormone taps into brain chemistry, so feeling emotional comes with the territory.
Some side effects don’t get talked about as much, even though they pop up in enough people to matter. Tender breasts make daily life a bit more uncomfortable, not just for women but also for anyone taking progesterone in gender-affirming care. Nausea and occasional vomiting can hit, pushing folks to skip meals or nibble on crackers all day.
There’s also weight changes—not always big ones, but enough to notice after a few weeks. Sleep troubles tie in with everything else, and restless nights lead to groggy days. Acne can flare up, especially in folks already dealing with breakouts. Not all side effects play out for everyone. Sometimes a person only sees one or two on the usual list.
Most people stick with mild symptoms, but not all side effects stay small. Some need immediate attention. Shortness of breath, sudden chest pain, unexpected swelling in the legs—these aren’t symptoms worth ignoring. Blood clot risk goes up slightly with hormonal medicines, according to studies published by the National Institutes of Health. Women with past clotting problems or high blood pressure should bring up those histories early and often with their doctor.
Most side effects ease up as the body gets used to the new hormone levels, but people don’t have to just tough it out. Adjusting the dosage or switching up how to take it—oral, cream, injection—sometimes cuts down on problems. If nausea hits, taking progesterone with food can ease the stomach. Simple things like adding more fiber to fight constipation or choosing a comfortable bra for breast soreness also go a long way. Checking in often with the doctor matters most, especially if any symptoms get worse or start to worry you. If the risks stack higher than the benefits, it makes sense to look into other treatment options that feel safer or less disruptive.
If you’ve ever cracked open a chemistry textbook or worked in a research lab, you’ve likely seen Pregnan-3,20-Dione pop up—better known in some circles as progesterone. This isn’t some shelf-stable kitchen spice; its value depends a lot on proper handling and careful storage. Years spent working with sensitive lab supplies taught me that tiny lapses can ruin months of prep work, waste budgets, and put studies at risk.
Exposure to light, heat, and humidity spells trouble for many organic compounds. Pregnan-3,20-Dione is no different. A friend once told me about a batch left near a sunlit window—within weeks, the results skewed and a lot of data ended up in the trash. Keeping this compound away from direct sunlight isn’t just smart; it’s essential. Most research facilities tuck it away in a dark cabinet, or better yet, in an amber glass bottle that blocks UV light.
For many years, I’d get that sinking feeling every time someone left a temperature-sensitive bottle sitting on a warm benchtop. Pregnan-3,20-Dione won’t last long at room temp if your room turns tropical. Store it in a cold spot—refrigerators set around 2 to 8°C typically do the trick. Avoid freezer burn; extreme cold can sometimes crack containers or introduce condensation later. Humidity seeps into unsealed bottles, clumping powders and turning crystals mushy. Always check caps and close everything tightly after use.
Too many labs run into problems because nobody knows what’s in a mystery vial. I still remember finding a dusty, unmarked bottle at the back of a fridge, nobody owned up to it, and it went straight to hazardous waste. A neat label—date received, date opened, and the lot number—saves headaches if something goes wrong or if you need to trace material back to a specific supplier.
Stashing Pregnan-3,20-Dione alongside strong acids or bases won’t win you points for safety. These chemicals tend to mess with each other, sometimes causing breakdowns or dangerous reactions. I learned that lesson the hard way after a fumes incident in a shared cabinet—scared everyone nearby and forced a costly evacuation. Separation from all reactive agents adds another layer of protection, and stops cross-contamination.
Even outside the lab, people working with raw hormone profiles need to use caution. Home chemists might overlook the risks of improper storage until their product turns unusable. If you’re not keeping Pregnan-3,20-Dione out of reach of curious kids or pets, you’re inviting trouble no one needs. Locking it up isn’t just about rule-following—it’s real safety.
Great storage starts with a habit. Put away what you use, close every container snug, and keep storage spaces clean. Get a cheap digital thermometer for your fridge, use those little desiccant packs to eat up moisture, and write clear labels for the next person. Proper care may seem like nitpicking, but it keeps you from repeating the same mistakes that cost researchers and pharmacies everywhere. These steps hop over a lot of preventable pitfalls, save time, and make sure all that investment doesn’t go out the window with your next spoiled sample.
Pregnan-3,20-Dione shows up in science textbooks as the official name for progesterone. In medicine, people hear about progesterone all the time, especially those going through fertility treatments or dealing with hormone imbalances. It's a key ingredient in a lot of hormone therapies, and gynecologists have used it to help with issues like irregular menstrual cycles or certain menopause symptoms. Still, most people just stick to calling it progesterone, probably because pregnan-3,20-dione sounds a bit intimidating.
In the United States, getting pure progesterone, or pregnan-3,20-dione, almost always means lining up a prescription. The FDA keeps it under prescription-only status since hormones play a major role in the body and even small changes make a difference. People sometimes stumble on supplements at vitamin shops that claim to be “natural progesterone,” but that stuff rarely matches pharmaceutical-grade hormones. Pharmacies and doctors work together for good reason here – the risks around dosing mistakes, unexpected side effects, and interactions with other medicines all add up quickly when hormones come into play.
It can tempt some folks to look for alternatives online, but grey-market sites or “compounded” versions from unlicensed sources often carry contamination risks. Getting the dose wrong doesn’t just make the treatment less effective – it could lead to blood clots, changes in mood, or create bigger hormonal messes down the line. A doctor’s supervision, at least in my experience, isn’t just about red tape. I’ve had relatives take progesterone for reproductive reasons, and the process needed real monitoring. Doses changed more than once, and the doctor always checked for possible side effects at each visit.
The prescription requirement didn’t appear out of thin air. Pregnan-3,20-dione plays a starring role in cycles and fertility, but throw it into the wrong hands or use it without good reason, and problems pop up. Some people look to progesterone creams for anti-aging or to counteract other health problems, not realizing the risks attached to self-dosing. Too much, and blood draws start showing liver strain or bad cholesterol. With too little, symptoms don't change, and frustration builds.
Hormones don’t act alone. Introducing new levels changes how other hormones act in the body, and the results don’t follow a script. I’ve seen strong personalities get more irritable, or usually calm folks develop sudden anxiety after starting on hormone treatments. This kind of change feels alarming, and it deserves a clinician’s attention. Rules aren’t about blocking access; they push for some common sense and careful supervision.
People wishing for easier access should push for better conversations with their healthcare providers. If someone believes they truly need pregnant-3,20-dione for unexplained symptoms, describing everything—sleep patterns, mood changes, energy swings—gives a full picture. I’d stress the value in partnering with doctors who actually listen, not just those who write scripts. For the folks clearly in need, regular monitoring—blood tests, check-ins, adjustments—reduces the risk of complications. Legislators and agencies reviewing these requirements should invite more patient voices, but should not trade safety for convenience. It's not about putting up walls. It's about protecting people from disasters they can’t see coming.
Pregnan-3,20-dione goes by a more familiar name in most doctor’s offices: progesterone. While folks tend to lump all hormones together, every one of them acts a little differently in the body. So, any question around “what dose should I take?” ends up being a big one. With Pregnan-3,20-dione, it’s a question that’s never been as simple as a one-size-fits-all answer.
If a doctor hands out a prescription for this hormone, he or she looks at where the patient stands today. Are they struggling with fertility? Fighting uterine bleeding that just won't quit? Managing menopause sweats? Each of these situations pulls the dose in different directions. Fertility clinics, for example, often prescribe anywhere from 100 to 200 mg per day, usually given as a vaginal suppository, oral capsule, or sometimes an injection. On the other hand, women handling menopause-related issues usually find themselves on lower oral doses—typically 100 mg to 200 mg daily, taken at bedtime.
Doctors learned long ago to tread carefully with hormones. Too little makes the treatment pointless, but too much sets off other health alarms. Researchers have tied high doses of pregnenolone-derived hormones to dizziness, mood changes, and sleep disruption. Plus, dosing up on progesterone without considering estrogen levels can bring a fresh batch of health headaches, like an increased risk of clots or even certain cancers. These aren’t theories—they turn up in clinic notes across the country every year.
People may read about progesterone creams or “natural” supplements in wellness forums. Many of these contain pregnan-3,20-dione or its close chemical relatives. These creams rarely tell the full truth about how much active ingredient gets absorbed into the body. My own family’s run-in with this came when my aunt tried over-the-counter progesterone for night sweats, hoping to skip a doctor’s visit. Two weeks later, she found herself groggy with wild mood swings. Her doctor—unsurprised—explained that over-the-counter creams can be a wild card. Your skin may not absorb what the label says, and without a lab test, how would anyone know their hormone levels in the first place?
Doctors watching over hormone therapy usually call for regular check-in visits. This monitoring isn’t just red tape. After starting or adjusting dosage, blood levels or at least a symptom check can catch problems before harm sets in. Trustworthy clinics also help patients understand the tradeoffs: weighing the risks of side effects, tracking for signs of blood clots, reviewing health history for cancer or liver disease, and sorting out drug interactions. Patients who press for answers and take time for those check-ins tend to land in a safer spot.
Insurance companies and pharmacies sometimes step between the doctor and patient with their own protocols or pre-approval hurdles. This tangles up the process even more, especially when a generic isn’t available or compounding is needed. Patients shouldn’t shy away from asking their pharmacist for extra information when a prescription gets filled. If a patient’s local pharmacist can’t help, the next step should be to call the prescribing doctor before taking the first dose. Real-world experience tells me that a minute of double-checking beats days of side effect worries.
No small pill, cream, or injection solves complicated hormone problems overnight. Quality guidance depends on real knowledge about Pregnan-3,20-dione and honest talk with a healthcare provider. People who respect what their body needs—and stay curious about their treatment—skip a lot of unnecessary health drama. A tailored, regularly reviewed plan stands out as one of the safest ways forward.
| Names | |
| Preferred IUPAC name | 17β-**Hydroxypregn-4-en-3-one** |
| Other names |
Progesterone β-Pregnane-3,20-dione P4 Δ4-Pregnene-3,20-dione |
| Pronunciation | /ˈprɛg.næn θriː ˈtwɛnti daɪˈoʊn/ |
| Identifiers | |
| CAS Number | 53-03-2 |
| Beilstein Reference | 1461086 |
| ChEBI | CHEBI:17026 |
| ChEMBL | CHEMBL730 |
| ChemSpider | 5236 |
| DrugBank | DB00396 |
| ECHA InfoCard | DTD ID: 100.000.136 |
| EC Number | 1.3.99.4 |
| Gmelin Reference | 8931 |
| KEGG | C00410 |
| MeSH | D011374 |
| PubChem CID | 6380 |
| RTECS number | KJ5510000 |
| UNII | 4G7DS2Q64Y |
| UN number | UN2811 |
| CompTox Dashboard (EPA) | DTXSID3023863 |
| Properties | |
| Chemical formula | C21H30O2 |
| Molar mass | 314.47 g/mol |
| Appearance | White crystalline powder |
| Odor | Odorless |
| Density | 1.12 g/cm³ |
| Solubility in water | Insoluble in water |
| log P | 2.98 |
| Vapor pressure | 2.48E-6 mmHg at 25°C |
| Acidity (pKa) | 12.97 |
| Basicity (pKb) | 3.20 |
| Magnetic susceptibility (χ) | -98.7e-6 cm³/mol |
| Refractive index (nD) | 1.045 |
| Viscosity | Viscosity: 8.03 mPa·s |
| Dipole moment | 2.52 D |
| Thermochemistry | |
| Std molar entropy (S⦵298) | 404.6 J⋅mol⁻¹⋅K⁻¹ |
| Std enthalpy of formation (ΔfH⦵298) | -93.01 kJ/mol |
| Std enthalpy of combustion (ΔcH⦵298) | -7227.9 kJ/mol |
| Pharmacology | |
| ATC code | G03DA04 |
| Hazards | |
| Main hazards | May cause respiratory irritation. May cause drowsiness or dizziness. |
| GHS labelling | GHS07, GHS08 |
| Pictograms | GHS02,GHS07 |
| Signal word | Warning |
| Hazard statements | H315: Causes skin irritation. H319: Causes serious eye irritation. H335: May cause respiratory irritation. |
| Precautionary statements | P201, P202, P210, P264, P280, P308+P313, P405, P501 |
| NFPA 704 (fire diamond) | 1-0-0 |
| Flash point | 161.8°C |
| Autoignition temperature | 410 °C |
| Lethal dose or concentration | LD50 (rat, oral): 10000 mg/kg |
| LD50 (median dose) | 4570 mg/kg (rat, oral) |
| NIOSH | SN7X8K56ZZ |
| PEL (Permissible) | PEL (Permissible) of Pregnan-3,20-Dione: Not established |
| REL (Recommended) | 0.02 – 0.20 µg/mL |
| IDLH (Immediate danger) | IDLH: 400 mg/m3 |
| Related compounds | |
| Related compounds |
Progesterone 17α-Hydroxyprogesterone Hydroxyprogesterone caproate Desoxycorticosterone Cortisone Cortisol |